OUR TECHNOLOGY MAKES USING A RETAIL PHARMACY SOLUTION TO SUPPORT CARE DELIVERY EASY TO IMPLEMENT AND MAINTAIN.
Enabling a Faster Response
Advanced Technology
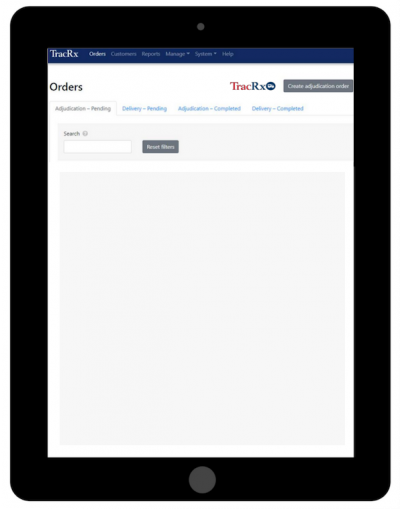
Our pharmacy benefit management processing platform administers your unique program rules and plan design, ensuring that medications processed at the pharmacy include the same level of review as an in-house pharmacy solution.
Our technology makes using a retail pharmacy solution to support care delivery easy to implement and maintain.
A Parameter-driven PBM Platform:
Plan Design Feature |
Service Description |
Formulary Management |
We load client formularies into our system. Formularies can be applied at the group level or down to an individual level. |
Max Allowable Paid |
Each plan can be set up with a maximum allowable paid limit, as well as rules to handle these scenarios, such as requesting a prior authorization (PA). |
Prior Authorization |
Formulary or other plan design rules can be set up to support PA protocol. Custom messaging at the POS is used to inform pharmacies who to call to request a PA. |
Authorized Physician Lists |
Authorized prescriber lists can be loaded into the system, along with rules for how to handle these scenarios, such as post and pay, pend and post (require PA) or deny. |
Refill, Quantity Limits, Days Supply |
Parameters can be put in the system to manage refills, days supply and quantity limits. |
Reporting
With a comprehensive suite of reports, we provide you with detailed information about your program utilization and spending. Importantly, we use these reports to discuss opportunities to lower your costs and identify how best to utilize backup services.
Data Security
As part of our commitment to data security, our systems have obtained HITRUST CSF-certified status. This certification demonstrates that the application has met key regulations and industry-defined requirements and is appropriately managing risk. Read our press release to learn more.

